Orthodontic treatment isn’t particularly risky, but as with any intervention to your body, it does carry some minor risks.
Whether you’re looking into orthodontic treatment for your child, or you’re considering treatment options as an adult, it’s important to have the information to be able to weigh up the risks and benefits of treatment before making a decision.
Toothache and mild discomfort
When you first start treatment, you may feel some mild discomfort as your mouth gets used to the orthodontic equipment and your teeth begin to move. This discomfort will vary from person to person, and will depend on your own pain threshold and the treatment you have chosen.
If you feel any discomfort due to the pressure on your teeth, we recommend taking over-the-counter pain relief.
Scratches and ulcers
At the start of your orthodontic treatment, it’s fairly common to feel some small scratches and ulcers on the inside of your mouth, especially if you’re wearing a fitted device such as braces. This will usually only happen for a couple of days, until your mouth gets used to the shape of your braces.
However this can be easily solved using orthodontic wax, which is an easy and immediate way to protect your mouth during this initial phase.
Gum infection
Maintaining good oral hygiene is important for everyone, but it’s especially important if you’re undergoing any type of orthodontic treatment. Poor oral hygiene can lead to gingivitis and gum infection which can slow down the movement of your teeth – if you’re wearing an orthodontic appliance then this can mean treatment takes longer. In some cases, the infection can cause irreversible damage to the tissues which support your teeth.
Make sure you maintain a healthy oral hygiene routine and follow the guidance of your orthodontist to prevent gum infections. Regular professional cleans with your dentist will also help.
Enamel demineralisation
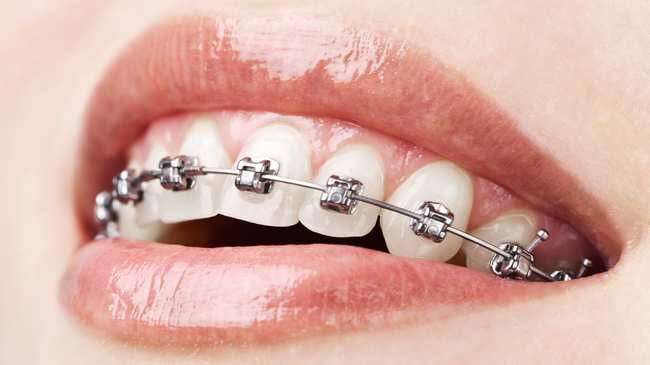
Enamel demineralisation, where the enamel wears away on the tooth, can occur during orthodontic treatment, particularly with fixed appliances such as braces. It is primarily caused by sugar, which starts a decay process in the enamel. If left to progress, over time this demineralisation can lead to cavities and tooth decay, which appears as white or yellow stains on the teeth.
Root shortening
For some patients, the length of the roots of their teeth become shorter during treatment. It’s nearly impossible to predict whether or not it will happen to you – but some people are more prone to it than others. In general, root shortening doesn’t have significant consequences, but on very rare occasions it may threaten the longevity of the tooth.
Tooth vitality
As orthodontic treatment moves the teeth, some pre-existing conditions (such as trauma or decay) might be aggravated by wearing an orthodontic appliance. The movement the tooth undergoes during treatment might further aggravate the tooth. While very rare, this can lead to the tooth becoming discoloured or requiring root canal treatment.